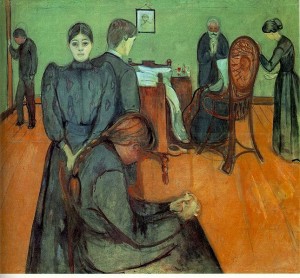
The Gold Standard for an Obscene Death.
 There is a sense in which publication of this letter in the Daily Telegraph was as inevitable as death itself.
There is a sense in which publication of this letter in the Daily Telegraph was as inevitable as death itself.
I have been waiting for it, or something like it, to appear since last October when the full function of The Mental Capacity Act 2005 came into operation.
None of us want to think of death, none of us want to discuss it, least of all, apparently, journalists, ancient superstition perhaps; and that is probably why one little known clause in the Act has received virtually nil publicity.
The Act, which was fan fared, to the small amount it was, was described as ‘empowering’ – now you could choose what medical treatment that you had – note, and note well, not wished to have, but had, at the end of your life. You cannot actually force the medical profession to give you any particular treatment, but you can refuse to have treatment. Hence, all the Act actually ‘empowered’ you to do, was to refuse treatment. If you had not taken advantage of the ability to ‘empower’ yourself by signing a Lasting Power of Attorney, enabling a chosen person to refuse treatment on your behalf, then the Act had cunningly hidden about its person, the ability to use the Court of Protection to appoint an ‘officer of the court’ – a civil servant or even a solicitor whom you had never met – to, if it decided that you did not have the Mental Capacity to do so yourself, for reasons varying from a congenital inability to understand, to perhaps being unconscious, to refuse that treatment on your behalf.
What the Act never did spell out, was that in England and Wales, food and water administered by a Doctor counts as ‘medical treatment’.
Dying of malnutrition – starvation – or lack of hydration – extreme thirst – is a painful and obscene manner in which to die. It has now become the ‘gold standard’ in end of life care. It has come about because as a nation we refuse to discuss euthanasia or assisted suicide in a reasonable or responsible manner. We become both emotional and obscurist, hiding our true views behind a cloak of carefully crafted language.
The original Lasting Power of Attorney Act came about because accountants and solicitors were alarmed that when their elderly clients became confused they might not be acting legally on their behalf. It didn’t come about because anybody wanted to ‘empower’ elderly and confused old ladies.
The Mental Capacity Act 2005 has been enlarged and updated to include medical care for similar reasons – to provide legal cover for Doctors and Nurses to take the actions they have always taken; but because we wouldn’t allow an honest debate regarding euthanasia or assisted suicide, it took the only route open to it – that of empowering Doctors to follow the ‘Bland‘ formula, and starve you to death when you were no longer economically sustainable.
Read this letter, study the statistics – 16.5 per cent of deaths, and resolve not to shut your mind to the subject this time. It will be you next, it will be someone close to you next, and we only have ourselves to blame for ignoring the subject. It won’t go away, that is inevitable.
SIR – The Patients Association has done well to expose the poor treatment of elderly patients in some parts of the NHS (report, August 27). We would like to draw attention to the new “gold standard” treatment of those categorised as “dying”. Forecasting death is an inexact science.
Just as, in the financial world, so-called algorithmic banking has caused problems by blindly following a computer model, so a similar tick-box approach to the management of death is causing a national crisis in care.
The Government is rolling out a new treatment pattern of palliative care into hospitals, nursing and residential homes. It is based on experience in a Liverpool hospice. If you tick all the right boxes in the Liverpool Care Pathway, the inevitable outcome of the consequent treatment is death.
As a result, a nationwide wave of discontent is building up, as family and friends witness the denial of fluids and food to patients. Syringe drivers are being used to give continuous terminal sedation, without regard to the fact that the diagnosis could be wrong.
It is disturbing that in the year 2007-2008, 16.5 per cent of deaths came about after terminal sedation. Experienced doctors know that sometimes, when all but essential drugs are stopped, “dying” patients get better.
P. H. Millard
Emeritus Professor of Geriatrics University of London
Dr Anthony Cole
Chairman, Medical Ethics Alliance
Dr Peter Hargreaves
Consultant in Palliative Medicine
Dr David Hill
Fellow of the Faculty of Anaesthetists of the Royal College of Surgeons
Dr Elizabeth Negus
Lecturer, Barking University
Dowager Lady Salisbury
Chairman, Choose Life
-
1
September 3, 2009 at 11:23 -
If the time comes, it’s a one-way ticket to Switzerland for me, and my relatives will have all the necessary instructions – ain’t nobody’s business but mine.
-
3
September 3, 2009 at 12:58 -
Allowing someone to die from dehydration is hideous & obscene – I know how uncomfortable I feel just when I get thirsty. God preserve us all from dying in the caring hands of the NHS – murder to order but without the decency to allow honest & open discussion on euthanasia. Gordon Brown – you have a lot to answer for.
-
4
September 3, 2009 at 14:01 -
As per usual, circumstances alter cases. If you consider the case of somebody in a coma from which they won’t emerge, who is going to die very soon from an intractable condition, but who is otherwise physically healthy, what’s to gain by prolonging the life of their body?
-
6
September 3, 2009 at 14:41 -
…”in England and Wales, food and water administered by a Doctor counts as
-
7
September 3, 2009 at 17:49 -
Thanks for breaking this “Nil By Mouth/Nil By Media” silence.
-
9
September 3, 2009 at 18:14 -
Really? I thought it was rather Bland myself …
-
10
September 3, 2009 at 18:56 -
From your post:
‘… The Mental Capacity Act 2005 has been enlarged and updated to include medical care for similar reasons -
12
September 3, 2009 at 20:20 -
Ever more totalitarian. As you point out who will be next to have their lives deemed not worth living?
We release those convicted of terrorist attrocities on the grounds of compassion, but murder those in most need of compassion.
Brown’s Britain.
-
14
September 3, 2009 at 22:12 -
Hi all, I’m a junior doctor working in the NHS- I have some practical experience with the issues you raise and I’d like to clarify a couple of points.
Firstly, the Mental Capacity Act is essential in some limited circumstances. As an example- an elderly gentleman who is increasingly confused with Alzheimer’s Disease. The Act enables him to make informed decisions about his care whilst he still has capacity to comprehend the situation, and to have these decisions respected in the future with his enduring power of attorney.
It is also useful to enable medics to make a decision in a patients best interests if they are unable to decide for themselves. Again as an example, this commonly occurs with elderly people with dementia who are admitted from home and unable to cope on their own anymore. They may be unable to give informed consent to be moved to a residential home and in this instance we would apply to the Court to nominate a third party to make decisions in the best interests of the patient. (assuming they have no next of kin). The Act allows a safe and transparent method of making difficult decisions in difficult circumstances.
With regard to the Liverpool Care Pathway (LCP), I completely disagree that we are doing patients a disservice in their last days by using his protocol.
A patient must fulfil stringent criteria to be placed on the LCP. The idea is that we do everything we can to give a patient a peaceful and dignified death. It is only used when the clinical prognosis is very poor ie less than a couple of days usually, and that they are unable to eat/drink safely or are unconscious (there are other inclusion criteria these are examples).
A patient isn’t simply left to rot, they are evaluated at a minimum of every 4 hours to ensure they are comfortable, pain free and that any symptoms are being dealt with. Yes, they often have a syringe driver because that is the least invasive to administer medications in semi-conscious people. To clarify a syringe driver may have any medicines in it, in a palliative setting this would commonly include anti-nausea drugs and pain killers which are titrated to effect.
I would disagree that we are inhumanely starving people- if they are unconscious then of course we won’t feed them. The average time a patient is on the LCP at my hospital is 23 hours before death- unlikely to be long enough to inflict the kind of suffering you describe. Additionally in the vast majority of instances, giving fluids will only delay death by a very short period.
I wholeheartedly agree with the line in the published letter ‘Experienced doctors know that sometimes, when all but essential drugs are stopped,
-
16
September 4, 2009 at 09:25 -
This is akin to the liitle form with the red crosses introduced by the Nazis which allowed doctors to select disabled children for extermination.
I am appalled. I thought a consequence of our going to war (70 years ago) was to stop states doing this sort of thing?
-
17
September 4, 2009 at 15:24 -
OK Anna, I’ll be specific. Almost three years ago, my younger daughter, who had been diagnosed ten years earlier with a brain tumour, entered a hospice. She knew she was dying, and she knew how it would happen (and it turned out to be an accurate prediction). This was a known one-way journey.
She entered a coma, from which she would definitely not regain consciousness.
You’ll be able to work out the rest for yourself – I’ll settle for assuring you that there was nothing whatever useless about my daughter during her life. -
19
September 4, 2009 at 17:08 -
Anna –
My daughter made a living will that contained her wishes for what should happen where she was unable to participate in decisions, and this was respected by those caring her.
Had there been an option for her to take the initiative, I do know she would have done so, but she was also minded about those who would have been affected.
Against the prevailing legal context, I can’t imagine her having been cared for better than was the case. She wasn’t going to regain consciousness, but there was nothing at all officious about her treatment. -
20
September 6, 2009 at 19:32 -
Allegoricus
I’ve been reading through the exchange of messages here. I’m desperately sorry for your loss and hope that you’ve found some little consolation between the loss of your daughter and now.
Anna
I’m in agreement with you on the current legally allowable method of allowing someone to die through malnutrition. I’ve been ill for years and would never allow the medical profession to starve me in the event that I am unable to make my own decisions so I’ve made a living will.
-
22
October 19, 2009 at 15:59 -
Dr. Peter Hargreaves, one of the writers of the Daily Telegraph Letter, contacted me to say he had ‘grave concerns about where Palliative Care was going in the UK’.
My father Thomas Milner – Case No. 6 of the Patients Association Report (http://www.patients-association.org.uk/) was NOT on the LCP – Liverpool Care Pathway.
He did NOT receive enough medication and went to his death twisting and turning, pulling at the sheets (this written in the Medical notes), with tears coming down his face.
The Palliative Care Consultant had failed to titrate (gradually increase) the amount of morphine in his syringe driver.
Palliative Care/MacMillan nurses wouldn’t give him anything 2 hours prior to death. We had to call G.P. to summon some help and a Junior Doctor arrived, doubled the dose in the syringe driver and Thomas Milner died 1 hour later.
The syringe driver from set up to death (55 hours) held ONLY 10mgs. morphine which the Healthcare Commission found to be ‘low in the circumstances’. The doubling of the dose (to 20mgs. )is NOT standard Palliative Care Practice.
I don’t think they really know what they are doing. Death like Birth cannot be endured according to ‘guidelines’ or ‘in vogue’ thinking!
God Help us All and Shame on Them!
-
23
October 19, 2009 at 16:05 -
http://www.tomsanguish.com is a dedicated site to Thomas Milner – Case No. 6 – Patients Association Report.
You can see the factual details taken from the Medical Notes.
Now Sir Andrew Cash OBE, Chief Executive of the Sheffield Teaching Hospital Trust Foundation has sent a letter to the Family of Thomas Milner nearly 4 years after his death.
Sir Andrew lists the time of set up and refill of the syringe driver which are INCORRECT – we have the Medical Notes!
He has upto now failed to acknowledge his errors. They are hiding.
Gross Errors were made.The system is CORRUPT!
-
24
April 20, 2010 at 23:49 -
Thank you Ana for your excellent article. So many people do not know about this pathway and the ways in which it can be applied inappropriately. A close relative, aged 80, suffered a stroke and the consultant was about to use the LCP. A stroke is not necessarily a terminal condition, nor was my relative in pain. We were horrified. We complained to both the consultants and hospital management. They seemed to pay attention to our complaint re the LCP. He was not fed enough intravenously though and became weaker. A law should be passed preventing doctors from using the LCP unless a patient requests sedation. As it stands, the UK is breaking the Human Rights Act (2005). The law society has championed the upholding of the Cochlan ruling for patients who are forced to fund their own care. They have more than enough material to bring a case regarding the LCP issues raised here.
{ 1 trackback }

{ 24 comments }